Diaphragmatic Breathing: A Clinical Tool for Occupational and Physical Therapists
This topic was reviewed by Sonia R., licensed and registered Occupational Therapist with Outreach.
As physical and occupational therapists we are charged with creating the conditions for our clients to perform the daily tasks and activities of their lives at the highest level of safety and independence possible. Incorporating diaphragmatic breath work into our clinical work can support our clients’ by improving endurance, posture, and psychological well-being so that they can do the things they want and need to do.
Diaphragmatic breathing, also called belly breathing, is the natural state of breathing in all mammals when in a parasympathetic nervous system response or relaxed state.
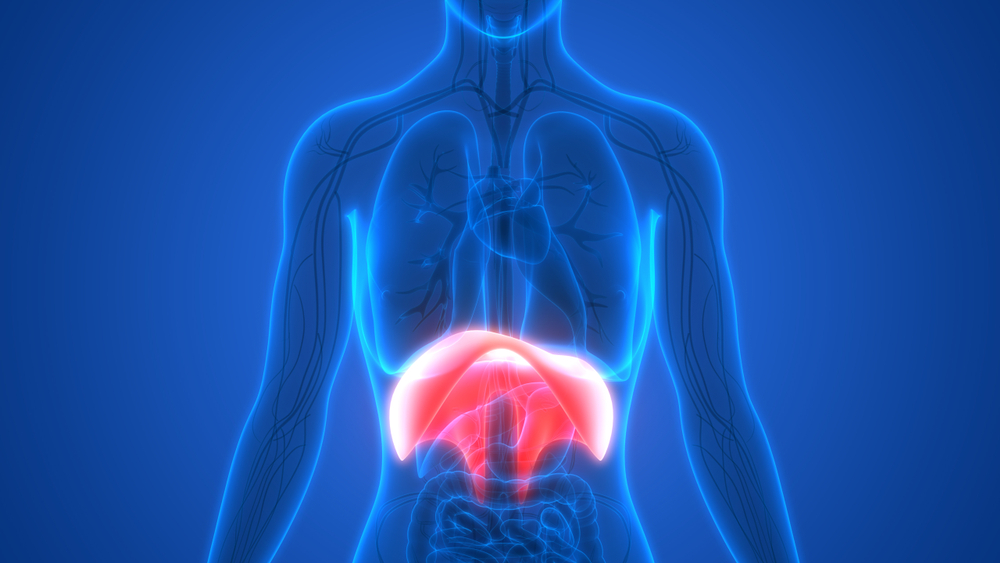
Diaphragmatic breathing occurs when the abdominal muscles assist the diaphragm, a large dome like muscle located horizontally at the base of the lungs, in contracting. During contraction the diaphragm moves down which causes the rib cage to expand. This expansion results in inhalation. When the diaphragm relaxes, it moves back up toward the lungs and exhalation occurs. It is a highly efficient and effective way to breathe.
Many of our patients have lived or currently live with high levels of stress and this, among other reasons, causes our patients to chest breathe, a pattern common in the sympathetic nervous system also known as the fight or flight response. In chest breathing, the muscles of shoulder and neck contract to lift the rib cage up and out creating some expansion. This bring the air outside the body in and the relaxation of these muscles releases the air back out. The muscles of the shoulders and neck do not have the ability to expand the ribcage to the same extent as the diaphragm and they also have much less endurance and are easily strained resulting in pain and tension in the neck and shoulders in people with this breathing pattern.
While we know that diaphragmatic breathing is the natural state of breath in parasympathetic nervous system response there is evidence that consciously doing diaphragmatic breathing can actually interrupt a fight or flight response and trigger a parasympathetic nervous system response. Because of this, it has been theorized that regular practice of diaphragmatic breathing can combat many of the symptoms associated with stress including high blood pressure, anxiety, depression, and chronic pain.
In addition to its effect on the nervous system and symptoms associated with stress, diaphragmatic breathing:
- Stretches and tones the abdominal and other core muscles
- Improves posture leading to increased independence and safety in transfers, ambulation, and ADLs
- Can play a role in curing pelvic floor disorders including incontinence[1]
- Improves pulmonary and cardiorespiratory fitness in people with COPD and Asthma[2]
- Reduces the subjective experience of chronic pain[3]
- Can assist in combating insomnia and sleep issues[4]
There are a number of ways to teach diaphragmatic breathing to a client. Before attempting to teach a client, the clinician should have a regular practice for themselves. A few techniques are described below.
- With client in a comfortable seated or reclined position, simply ask the client to place one or two hands on their belly. Ask the client to breath in through their nose and out through pursed lips. Instruct them to move the belly outwards with each inhalation and relax the belly back in on each exhalation. It may take multiple tries to get it. If they over-efforting, encourage them to do less or move on to a different technique.
- Sometimes imagery can help- again with client lying down or sitting up, ask the client to imagine their belly filling like a balloon on the inhale and deflating on the exhale.
- For some, a different hand position is more effective. With client in a seated position, ask the client to place hands on either side of the low rib cage, below the bra line. As they breath ask them to imagine their ribcage expanding/widening out into their hands as they inhale and narrowing on the exhale.
- This technique encourages slower, deeper breaths which requires engagement of the abdominals and diaphragm. Ask the client to count to 2-4 seconds on the inhale and 4-6 seconds on the exhale.
When the client is proficient in diaphragmatic breathing ask them to use the technique during exercises, transfers and other therapeutic activities. Often clients will feel that tasks are easier and less painful when done while attention is paid to the breath. Though it requires some effort and practice to learn a new pattern of breathing, over time diaphragmatic breathing will become automatic and feel natural.
Sources:
[1] Shaw, I.; Shaw, B.S.; Brown, G.A. (2010). “Role of Diaphragmatic Breathing and Aerobic Exercise in Improving Maximal Oxygen Consumption in Asthmatics”. Science & Sports. 25: 139–145. doi:10.1016/j.scispo.2009.10.003. Retrieved 2015-02-11.
[1] The Effect of Deep and Slow Breathing on Pain Perception, Autonomic Activity, and Mood Processing—An Experimental Study
H. Wennergren-B. Öberg – British Journal of Urology – 1995
Volker Busch-Walter Magerl-Uwe Kern-Joachim Haas-Göran Hajak-Peter Eichhammer – Pain Medicine – 2012
Mariano Chóliz – Perceptual and Motor Skills – 1995